Dementia
Dementia is the general term used to describe a progressive decline in cognitive function. This refers to a patient of normal intellect who is experiencing difficulties with thought and memory.
There are a number of potential causes of dementia. Many confuse the terms dementia and Alzheimer disease. Alzheimer disease is just one potential cause of dementia.
It is important to have a neurologist evaluate anyone experiencing difficulties with thought. While some of these patients with turn out to have Alzheimer disease, others may have a different explanation of their symptoms. Some causes of dementia are potentially curable, while others can be managed with medication. Some forms of dementia are resistant to therapy.
Several potential causes of dementia include:
Most types of dementia are nonreversible (degenerative). Nonreversible means the changes in the brain that are causing the dementia cannot be stopped or turned back. Alzheimer's disease is the most common type of dementia.Lewy body disease is a leading cause of dementia in elderly adults. People with this condition have abnormal protein structures in certain areas of the brain.
Dementia also can be due to many small strokes. This is called vascular dementia.
The following medical conditions also can lead to dementia:
- Parkinson's disease
- Multiple sclerosis
- Huntington's disease
- Pick's disease
- Progressive supranuclear palsy
- Infections that can affect the brain, such as HIV/AIDS and Lyme disease
- Brain tumors
- Changes in blood sugar, sodium, and calcium levels (see: Dementia due to metabolic causes)
- Low vitamin B12 levels
- Normal pressure hydrocephalus
- Use of certain medications, including cimetadine and some cholesterol-lowering medications
- Chronic alcohol abuse
Symptoms:
Dementia symptoms include difficulty with many areas of mental function, including:
- Language
- Memory
- Perception
- Emotional behavior or personality
- Cognitive skills (such as calculation, abstract thinking, or judgment)
Mild cognitive impairment is the stage between normal forgetfulness due to aging and the development of dementia. People with MCI have mild problems with thinking and memory that do not interfere with everyday activities. They are often aware of the forgetfulness. Not everyone with MCI develops dementia.
Symptoms of MCI include:
- Forgetting recent events or conversations
- Difficulty performing more than one task at a time
- Difficulty solving problems
- Taking longer to perform more difficult mental activities
- Language problems, such as trouble finding the name of familiar objects
- Misplacing items
- Getting lost on familiar routes
- Personality changes and loss of social skills
- Losing interest in things you previously enjoyed, flat mood
- Difficulty performing tasks that take some thought, but that used to come easily, such as balancing a checkbook, playing games (such as bridge), and learning new information or routines
- Forgetting details about current events
- Forgetting events in your own life history, losing awareness of who you are
- Change in sleep patterns, often waking up at night
- More difficulty reading or writing
- Poor judgment and loss of ability to recognize danger
- Using the wrong word, not pronouncing words correctly, speaking in confusing sentences
- Withdrawing from social contact
- Having hallucinations, arguments, striking out, and violent behavior
- Having delusions, depression, agitation
- Difficulty doing basic tasks, such as preparing meals, choosing proper clothing, or driving
- Understand language
- Recognize family members
- Perform basic activities of daily living, such as eating, dressing, and bathing
- Incontinence
- Swallowing problems
__________________________________________________
__________________________________________________
As part of the visit at Armstrong Neurology, we endeavor to provide comprehensive care and to address a wide variety of issues that frequently impact patients with cognitive impairment.
Issues that will commonly be addressed in patients who have cognitive impairment:
1. An overall care plan
- This will involve the patient, family members, and other caregivers
- Identification of a caregiver and individual with power of attorney for the patient
- Advanced care planning
2. Preventive care and screening
- Identification of factors that may put the patient at risk
- Evaluation of mood disturbances and depression
- Completion of the Beck Depression Inventory
- If indicated, a plan to address depression and other behavioral issues will be formulated
3. Staging of dementia
- Functional Assessment Staging Tool
- Dementia Severity Rating Scale will be completed annually at follow up visits
4. Cognitive assessment
- A number of assessment tools are available including formal neuropsychiatric testing
- Completion of the Montreal Cognitive Assessment
4. Cognitive assessment
- A number of assessment tools are available including formal neuropsychiatric testing
- Completion of the Montreal Cognitive Assessment
5. Functional status assessment
- An assessement of the patient's ability to perform basic and instrumental aspects of daily living
|
6. Neuropsychiatric symptom assessment This includes evaluation of potential activity disturbances: Agitation Wandering Purposeless hyperactivity Verbal or physical aggressiveness Resistiveness to care Apathy Mood disturbances: Anxiety Dysphoria Thought and perceptual disturbances: Having fixed false beliefs Hearing or seeing non-present entities (hallucinations) |
Socially inappropriate behaviors Appetite Eating disturbances Sleep disorders Diurnal / sleep-wake cycle disturbances Repetitive behavior / Impulsiveness Irritability Mood lability / fluctuations Euphoria Paranoia |
7. Management of neuropsychiatric symptoms
8. Counseling regarding safety concerns:
- A variety of options will be discussed to ensure patient safety
- Home safety evaluations may be ordered
- Supervision options will be considered
|
Fall risk Gait / balance Financial management Home safety risks (cooking / smoking) Suicidality Physical aggression Wandering |
Being left alone Inability to respond rapidly to crisis / household emergencies Driving Operation of hazardous equipment Abuse / neglect Access to potentially dangerous materials Access to firearms or other weapons |
9. Counseling regarding the risks of driving:
10. Caregiver education and support
- Extensive resources are available here on the Armstrong Neurology site
__________________________________________________
Resources to assist patients with dementia:
There a number of positive interventions that can be taken to help patients who are experiencing difficulties with their cognitive function. The more active and involved the patient is in various activities of daily living the better.
Many patients benefit from having an "activity table". Consider having a dedicated space for the patient. A large desk or banquet table would be ideal. This could be an activity area and personal space just for the patient. Items that could be included in this space might be; a personal computer / iPad, cell phone, activities, hobbies, puzzles, and games.
Here are some additional ideas that may be helpful:
There a number of positive interventions that can be taken to help patients who are experiencing difficulties with their cognitive function. The more active and involved the patient is in various activities of daily living the better.
Many patients benefit from having an "activity table". Consider having a dedicated space for the patient. A large desk or banquet table would be ideal. This could be an activity area and personal space just for the patient. Items that could be included in this space might be; a personal computer / iPad, cell phone, activities, hobbies, puzzles, and games.
Here are some additional ideas that may be helpful:
_____________________________________
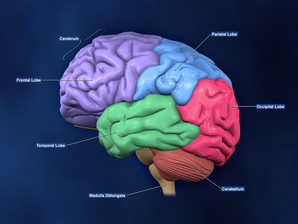
Imaging:
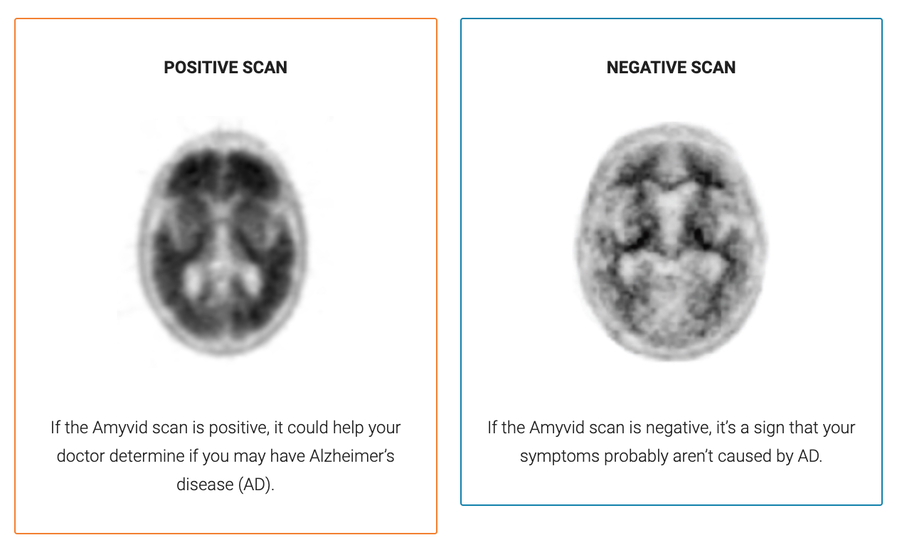
MRI or CT of the brain is part of the standard evaluation. Other imaging options such as the amyloid PET scan may be considered in certain circumstances.
MRI or CT of the brain is part of the standard evaluation. Other imaging options such as the amyloid PET scan may be considered in certain circumstances.
_____________________________________
CSF and plasma Abeta42/40 ratios:
These tests may be helpful as an adjunct to the diagnosis of dementia due to Alzheimer disease, but they have limitations:
"In theory, the results of these studies indicate that if ABeta42 were to be used in a specialist clinic in a group of 1000 people, where 520 (52%) have Alzheimer's dementia, an estimated 602 would have an ABeta42 result. This would indicate that Alzheimer's dementia is present. Of these, 192 (32%) would be incorrectly classified as having Alzheimer's disease. Of the 398 people with a result indicating that Alzheimer's disease is not present, 110 (28%) would be incorrectly classified as not having Alzheimer's disease. The included studies used different levels of ABeta42 to make the diagnosis of Alzheimer's disease, and the accuracy of the test depended on the level of ABeta42 used."
https://www.cochrane.org/CD010945/DEMENTIA_how-accurate-abeta42-test-distinguishing-alzheimers-disease-other-types-dementia-patients-seen
_____________________________________
Medical Therapy:
_____________________________________________________________________________
Internet Resources to assist in the care of patients with cognitive impairment:
_______________________________________________________________________________
|
Dr. Roger Rosenberg is a highly respected professor of neurology at Southwestern and was a mentor for Dr. Armstrong during his residency training. |
|
Link to the Alzheimer Association website:
_______________________________________________________________________________
_______________________________________________________________________________
Lewy body dementia
Lewy Body Dementia (also called Dementia with Lewy bodies) is a form of dementia that shares characteristics with both Alzheimer's and Parkinson's diseases. Lewy Body dementia (LBD) symptoms resemble other diseases but LBD is especially challenging to diagnose correctly.
As a caregiver, you may feel discouraged in the face of this dementia, however, you can make the life of someone with LBD safer and more comfortable. By more fully understanding LBD and by using strategies that help you can also bring more hope and purpose into your own life.
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________